Topic 2: What is a protein? What is GNAQ?
What is a protein?
I like to think about questions like this from a historical perspective. In the first half of the 1800s scientists tried to understand what our bodies are made of. The word “protein” was coined in 1838, and by 1850 about five proteins had been discovered. One was hemoglobin, the protein that carries oxygen in blood and includes a chemical group that gives blood its red color. Another was albumin. All the first proteins to be discovered were very abundant, making them easier to study. By the year 1900 it was appreciated that proteins are made up of amino acids. There are 20 main amino acids: we get half from our diet, and our bodies can manufacture the other half.
By the 1950s the first proteins were sequenced: each protein is a string of amino acids, typically with about 300 in a row (sometimes more, sometimes less). By the 1960s the genetic code was figured out, explaining how genes (DNA) can direct the synthesis of proteins.
We now know that people have about 20,000 genes that make proteins.
What is GNAQ?
Let me introduce you to a single protein called G protein subunit alpha q, abbreviated GNAQ (pronounced G alpha q). Each protein consists of a “string” of connected amino acids. Here’s the string of amino acids for GNAQ; there are 359 of them.
MTLESIMACCLSEEAKEARRINDEIERQLRRDKRDARRELKLLLLGTGESGKSTFIKQMRIIHGSGYSDE DKRGFTKLVYQNIFTAMQAMIRAMDTLKIPYKYEHNKAHAQLVREVDVEKVSAFENPYVDAIKSLWNDPG IQECYDRRREYQLSDSTKYYLNDLDRVADPAYLPTQQDVLRVRVPTTGIIEYPFDLQSVIFRMVDVGGQR SERRKWIHCFENVTSIMFLVALSEYDQVLVESDNENRMEESKALFRTIITYPWFQNSSVILFLNKKDLLE EKIMYSHLVDYFPEYDGPQRDAQAAREFILKMFVDLNPDSDKIIYSHFTCATDTENIRFVFAAVKDTILQ LNLKEYNLV
I got this information from an NIH website (https://www.ncbi.nlm.nih.gov/protein/40254462). Each letter is an abbreviation for an amino acid, such as R for arginine. I’ve highlighted the 183rd amino acid (an R) because that’s the one that changes to something else (to a Q) in Sturge-Weber syndrome.
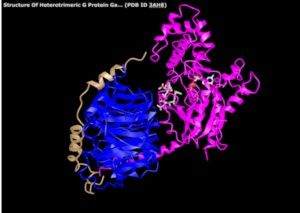
At the top of the article is a picture of the GNAQ protein (in magenta) along with two “partners” it binds to. Those partners are other proteins shaded blue and brown. The picture also shows a drug that inhibits GNAQ (the drug is in gray, embedded in the magenta; most drugs are small in size compared to proteins, and they’re usually not made up of amino acids as proteins are).
In the last post I mentioned that DNA and genes may seem abstract. It’s the same way with proteins; we may hear “you should eat protein in your diet” but we don’t actually see proteins. Unless you’re a biologist studying them. We can purify GNAQ so we have a test tube with pure protein. We can add a colorful “flag” so we can look at the protein inside a cell using a microscope. We can study its structure and function in tremendous detail.
What happens to GNAQ in Sturge-Weber syndrome?
In Sturge-Weber syndrome and in port-wine birthmarks, there’s a mutation in the GNAQ gene. When the gene makes its protein, one amino acid changes. The change is called R183Q: the R (arginine) at position 183 is changed to a different amino acid, Q (glutamine). Normally GNAQ acts like a switch that turns on and off. The effect of the mutation is that GNAQ is slightly turned on (“activated”) and kept on.
Now that we know this, we’d like to turn the switch back off. One way to do that would be to find a drug that turns it off. But we’d also need to lower the protein’s activity safely: If we turn it off in the wrong cell type, or turn it off too strongly, that could cause extreme problems.
Conclusions: the bigger picture
I’ve just introduced you to the GNAQ protein.
We know that, by chance, a mutation can happen in the GNAQ gene (Topic 1). We know that mutation results in a slightly changed protein (this post). That happens mostly in endothelial cells. In other posts I’d like to tell you a bit more:
· What an endothelial cell?
· What does it mean for GNAQ to be “turned on” (activated) and why does that matter?
· Can we engineer a person’s cells to fix the mutation?
All of this is meant to help us get close to figuring out treatments that can help treat the root causes of SWS.







