Glaucoma is an optic neuropathy characterized by a specific pattern of optic nerve head and visual field damage resulting from intraocular pressure (IOP) that is too elevated for the optic nerve to withstand.
In Sturge-Weber syndrome (SWS), glaucoma develops in about 70% of children who have involvement of the upper lid by the vascular malformation and eventually in nearly all those who have complete involvement of both the upper and lower lids. About one-third of such children have glaucoma within the first three years of life. This is due to localized high venous pressure and occlusion of the drainage system of the eye. In the other two-thirds, glaucoma manifests later during childhood or adulthood. In all cases, the fluid produced within the eye, the aqueous humor which nourishes the lens and cornea and maintains the shape of the eyeball, cannot get out of the eye easily, and the intraocular pressure which builds up results in slow, progressive optic nerve damage.
Symptoms of Glaucoma
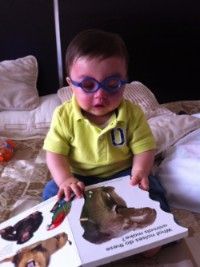
Often, glaucoma has no symptoms. In infants, however, glaucoma may be present with photophobia (increased sensitivity to light), tearing, and blepharospasm (intense squeezing of the eyelids to avoid bright stimuli). On cursory evaluation, signs of an enlarged cornea, which may also be hazy or opaque in appearance, are readily identified. In its early stages, however, most older children and adults with glaucoma will have no sensation or knowledge of the condition. Only in rare cases, when the intra-ocular pressure elevates to very high levels, may the individual may feel any discomfort.
An individual’s visual field becomes reduced over time once approximately half of the optic nerve has become damaged. It is thus important that glaucoma be detected and treated before extensive damage occurs.
Diagnosing Glaucoma
Tonometer: The tonometer is a device that directly measures the pressure of the fluid within the eye. After a few anesthetizing drops are placed on the eye, the tonometer is pushed lightly against it. The resistance rebound pressure of the eye against the tonometer provides a measurement of the internal pressure.
Visual Field Test: A visual field test is an important test to determine the extent of any damage to the optic nerve resulting in visual loss. The test measures an individual’s peripheral field of vision.
Ophthalmoscopy: An ophthalmoscope is a device that allows a physician to look at the optic nerve and retina through the eye’s pupil. By such examination, the physician may determine the extent of optic nerve damage.
Glaucoma Treatment
A number of steps can progressively be taken to treat glaucoma. Many patients respond well to simple procedures, such as topical eye drops which lower the intraocular pressure. However, where medication is not sufficiently effective, surgery may be required. In many cases, a combination of
surgery and some eye drops are required to help control glaucoma.
Medications
Medications consist of eye drops. Less commonly, inserts (wafer-like strips of medication that are placed in the corner of the eye), or eye ointments may be used.
Goniotomy (a surgical procedure in which the doctor uses a lens called a goniolens to see the structures of the front part of the eye (anterior chamber))
In this delicate operation performed in infants, a tiny blade is inserted through the cornea, across the anterior chamber, and in a sweeping motion, incises the trabecular meshwork (the drainage system of the eye), allowing the aqueous humor to flow more directly into Schlemm's canal without having to pass through an obstructive trabecular meshwork. The operation is performed under direct visualization using a special mirror called goniolens.
Trabeculectomy
This is an alternative to goniotomy and preferable when the cornea is hazy and precludes a view of the trabecular meshwork. An incision is made in the outer portion (scleral wall) of the eye until Schlemm's canal is reached. A tiny probe is inserted into the canal and rotated so that it breaks through the trabecular meshwork, allowing the aqueous humor to flow directly into Schlemm's canal. The results of goniotomy and trabeculectomy are about the same.
Trabeculectomy
This procedure is usually performed when goniotomy or trabeculectomy has failed. A trapdoor is made in the wall of the eye and a piece of trabecular meshwork is removed leaving a small hole. The trapdoor is sutured back partially closed and the aqueous humor flows through the small opening, forming a small blister-like deviation of the white conjunctival tissue which covers the sclera, called a filtering bleb. In infants and children, it may be performed with simultaneous administration of a drug to prevent excessive scarring, such as 5-fluorouracil or mitomycin-C at the risk of increasing the chance for infection.
Setons
Also known as valves, implants, shunts, or tubes. Often used if trabeculectomy has failed. A plastic drainage tube is inserted into the eye and connected to a reservoir sutured onto the wall of the eye.
Cyclodestructive Procedures
The ciliary body is located directly behind the iris and is covered by an epithelium that secreted the aqueous fluid. If filtration surgery fails to improve the outflow of aqueous from the eye, an alternative is to destroy a portion of the ciliary body epithelium in order to decrease the amount of aqueous fluid that is produced.
A portion of this aqueous-producing tissue may be destroyed by either freezing the tissue or burning it with lasers. Complications include overtreatment in a significant proportion of patients causing ocular hypotony which leads to loss of vision A more recent technique, endoscopic cyclophotocoagulation, involves inserting a laser and optical probe directly into the eye so as to better visualize and restrict treatment to only the ciliary body and not surrounding structures. Complications include cataract formation. Many surgeons still regard these procedures as a last resort.
Physician/Patient Follow-up
Glaucoma is a life-long risk in patients with SWS and port-wine birthmarks affecting the eyelids. Therefore, yearly examinations are advocated at a minimum. Initial screening of newborns with SWS should take place within the first three months of age. Follow-up examinations should be individualized for each patient and may occur as often as monthly in complicated cases. Frequent examinations under anesthesia may be required in small children and uncooperative patients.







